How The Brain Plays A Role In Rheumatoid Arthritis Inflammation
A new study from researchers at Michigan Medicine explores links between chronic joint inflammation and cognitive impairment.
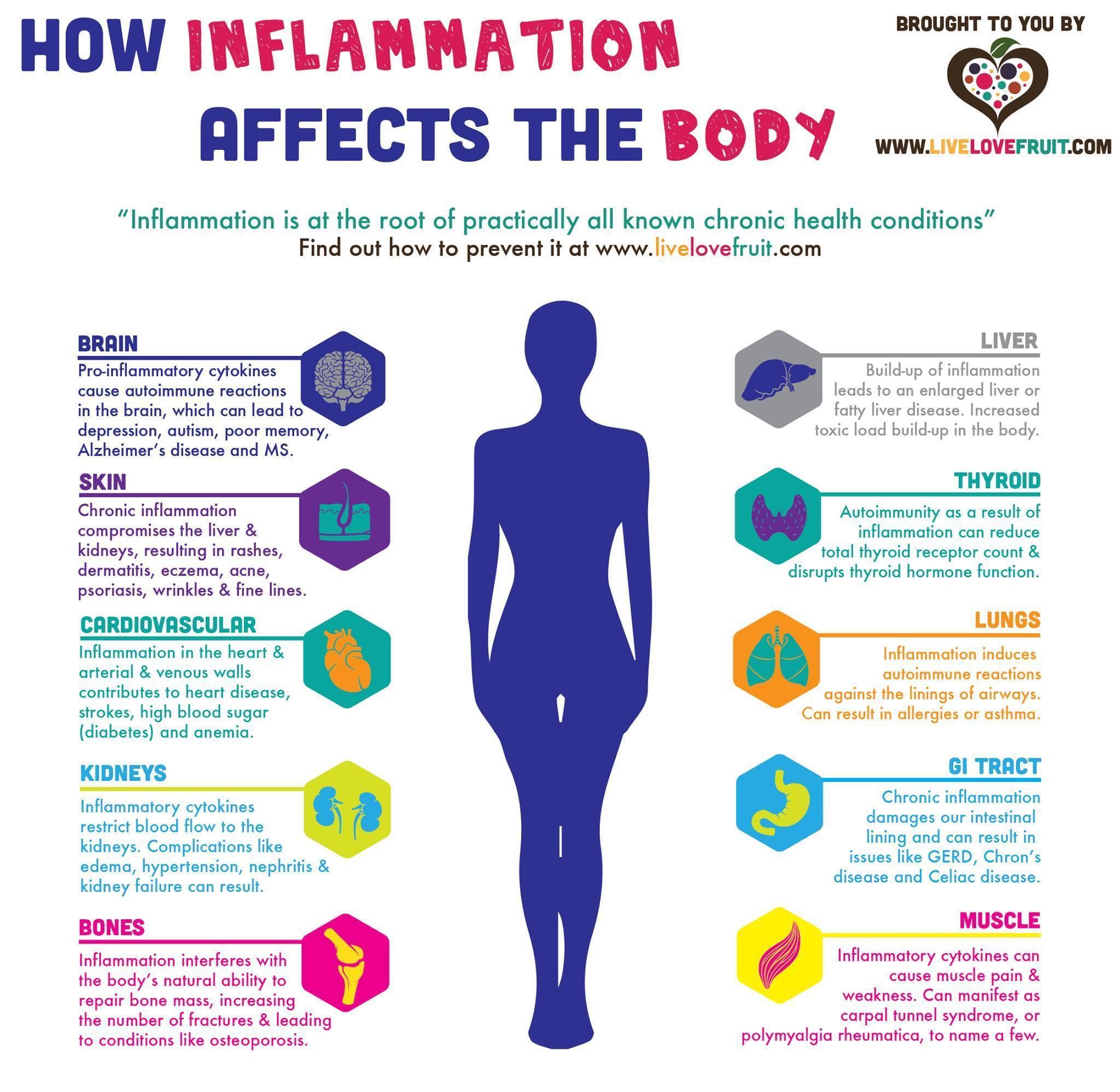
In patients with chronic inflammatory conditions, such as rheumatoid arthritis, there has been limited understanding of how this inflammation affects the brain.
LISTEN UP: Add the new Michigan Medicine News Break to your Alexa-enabled device, or subscribe to our daily audio updates on iTunes, and Stitcher.
A new study published in Nature Communications examines this issue.
Rheumatoid arthritis is an inflammatory and autoimmune condition with nasty levels of inflammation that can affect a persons joints and the rest of their body, inducing fatigue, sleep and creating cognitive difficulties, says Andrew Schrepf, Ph.D., a research investigator at Michigan Medicines Chronic Pain and Fatigue Research Center and one of the lead authors of the study.
Even though it has been assumed for a long time that the inflammation we see in blood is impacting the brain, up until this study we didnt know precisely where and how those changes in the brain were actually happening.
Schrepf says the effects of inflammation are more understood in short-term illnesses, but the same cant be said for chronic conditions.
What Are The Risk Factors For Brain Fog With Ra
Cognitive issues are complex. Because of this, the solution to brain fog may involve many factors. To lower your odds of developing cognitive issues, pay attention to risk factors like:
Lack of sleep. If you donât get enough sleep, you may not be able to think as well. Follow a healthy sleep routine that allows you to get around 8 hours of rest each night. Create a comfortable, dark, and cool bedroom environment. Cut computer screen time out before bed and stay away from caffeine later in the day.
The wrong medications. If youâre on conventional DMARDs or long-term corticosteroids, you may want to consider another medication. Talk to your doctor about these and other medications that may cause brain fog.
Low levels of physical activity. Exercise can improve your cognitive function. Create a workout routine to keep yourself consistent.
Control your mindset. If you have RA, itâs easy to get anxious about the future. But this stress takes up important brain space and could add onto any brain fog you already deal with. Focus on the present and work on habits that lower your anxiety levels.
You might also notice that your brain fog is more intense at certain points in the day. You may feel it more in the morning or when youâre stressed and tired. Keep a schedule that works well with your cognitive function. Complete the tasks that need more focus when your brain fog is at a minimum.
Inflammation Ra And Dementia
While both RA and dementia are partly due to a genetic predisposition, theres another underlying cause they share: inflammation. The chronic inflammatory process for rheumatoid arthritis can affect brain inflammation, due to hardening of the arteries, says Jonathan Greer, MD, a rheumatologist at the Arthritis & Rheumatology Associates of Palm Beach and an assistant clinical professor of biomedical sciences at Florida Atlantic University. This causes decreased blood to the brain, which can lead to vascular dementia.
While the Cureus review questioned whether RA medications such as disease-modifying antirheumatic drugs , including methotrexate, hydroxychloroquine, and sulfasalazine, may also lead to an increased risk of dementia, Dr. Greer cautions against reading too much into this. The underlying inflammation caused by rheumatoid arthritis may not be sufficiently controlled with these drugs, and, therefore, the inflammation itself could lead to the dementia, Greer says. Indeed, the association was not found with tumor necrosis factor agents and biologics, which are sometimes better at controlling inflammation.
No matter which treatment youre prescribed for RA, You should not be fearful, and you should never stop these drugs without your doctors permission, Greer emphasizes. If you have any concerns about your treatment, Work in a collaborative fashion with your doctor to find the best for you.
Also Check: How To Relieve Arthritis Pain In Neck
Which Patients With Rheumatoid Arthritis Get Vasculitis
Rheumatoid vasculitis most often occurs in people with at least 10 years of severe disease. In general, people who get vasculitis have many joints with pain and swelling, rheumatoid nodules, high concentrations of rheumatoid factor in their blood, and sometimes smoke cigarettes. They may also have an enlarged spleen and chronic low white cell count, a condition known as Felty’s Syndrome.
Fewer than five percent of people with rheumatoid arthritis get skin vasculitis. Fortunately, far fewer people get vasculitis of larger arteries.
There is evidence to support that since the introduction of effective treatments for rheumatoid arthritis, the occurrence of rheumatoid vasculitis is far less common.
The Nervous System And Arthritis Pain
Learn how pain information travels in the body through the nervous system and how arthritis treatments target specific areas to reduce pain.
The Nervous System and Arthritis Pain
There is no single pain center in the body. Your nervous system controls how you process and feel pain. The nervous system consists of two basic parts:
-
Central nervous system: the brain and spinal cord
-
Peripheral nervous system: nerves and nerve pathways throughout the body
When the body is damaged by disease or injury, tissues in the affected area release chemicals that communicate with nerves. Nerve pathways carry the messages from that area to the spinal cord and up to the brain. Pain information goes to several parts of the brain that recognize pain but also help control and adjust mood, sleep and hormones. Thats why having chronic pain can affect so many aspects of your body and daily life.
The brain sends messages back through the pathways down to the body to reduce or stop pain sensations. The message from the brain may also trigger an immediate response, for example, to pull your hand away from a hot stove.
Arthritis, pain relief treatments target your nervous system in a variety of ways:
-
Blocking or turning down pain messages in the brain
-
Stopping inflammatory chemicals from communicating with nerves
-
Quieting overactive nerves and/or blocking them from sending pain messages
-
Stimulating the release of natural pain-relieving chemicals called endorphins
Managing Pain
Read Also: Does Rheumatoid Arthritis Affect Your Lungs
Ask Your Doctor About Switching Medications
Most of the time, your recommended medication will help brain fog by easing the rest of your arthritis symptoms. But every now and then, steroid-based drugs like prednisone might cause side effects like brain fog, anxiety, and sleeplessness, says Dr. Blazer.
Dont ever stop taking a medication without checking with your doctor, or avoid one because of the slight risk of unpleasant side effects, but do keep in mind that finding the right arthritis drug might take some trial and error. If you suspect your medication is having a negative side effect, talk to your doctor about your options.
How Doctors Diagnose Arthritis Jaw Pain
The underlying causes for jaw pain can be hard for doctors to suss out, as the TMJ is a very complex joint with multiple factors affecting it. Your rheumatologist or dentist may recommend a specialist who deals with TMJ disorders, called an oral and maxillofacial surgeon. A thorough comprehensive evaluation and history taking is crucial to accurately diagnosing the etiology of jaw pain, Dr. Levi says.
Osteoarthritis is often diagnosed based on symptoms and imaging, and is commonly is associated with joint sounds, known as crepitus, Dr. Levi says. Osteoarthritis is also often associated with morning stiffness, jaw tightness, and decreased range of motion of the jaw.
Jaw bone and cartilage changes due to arthritis may be seen on imaging tests such as an X-ray, CT scan, or MRI. Changes that can be visualized on imaging include condylar beaking or flattening , and decreased joint space, Dr. Levi says.
Other forms of arthritis, such as rheumatoid arthritis, may be diagnosed with help from blood tests, Dr. Levi says. With inflammatory or autoimmune diseases, you will have elevated inflammatory markers like c-reactive protein or erythrocyte sedimentation rate many rheumatoid arthritis patients also test positive for antibodies such as rheumatoid factor and anti-CCP.
But if you have inflammatory arthritis, chances are jaw pain wont be your first symptom and if youve already been diagnosed, your doctor will have an indication that jaw pain may be due to your condition.
Recommended Reading: Can Psoriatic Arthritis Cause Anemia
Whats The Outlook For Someone Living With Arthritis
Since theres no cure for arthritis, most people need to manage arthritis for the rest of their lives. Your healthcare provider can help you find the right combination of treatments to reduce symptoms. One of the biggest health risks associated with arthritis is inactivity. If you become sedentary from joint pain, you may face a greater risk for cancer, heart disease, diabetes and other serious conditions.
Rheumatoid Arthritis Of The Cervical Spine
When you wake up to stiff joints compliments of rheumatoid arthritis , one becomes gallingly aware of each place the body bendsknuckle, knee, wrist and anklebut when the stiffness affects the atlantoaxial and atlanto-occipital joints in your upper neck, the cervical spine, the disease can turn dangerous. These joints, which pivot your head to look up, down, right and left, share neck space with the spinal cord and lie just below the brain stem. It is important to seek quick treatment to prevent swelling in this area and damage to these joints.
Rheumatoid arthritis can affect the neck joints causing stiffness and pain when moving your head up, down and/or side to side. Photo Source: 123RF.com.
Understanding your rheumatoid arthritis diagnosis and treatment options can help you comprehend your doctors game plans. Gaining knowledge about what can be done to manage the disease can also dissolve feelings of depression or isolation.
Patients who fare best make peace with the fact that RA is a lifelong condition that will alternately flare up and go into remission, says Wendy Chi, MD, Assistant Professor of Medicine in the Division of Rheumatology at Mount Sinai in New York City.
You May Like: Is Advil Good For Arthritis
Other Rheumatoid Arthritis Treatment Options
Patients can also relieve joint stiffness with like swimming, walking or cycling, Dr. Chi said. I generally prefer low impact, Dr. Chi stated. The more force you apply to the joints, the more damage you could do to the cartilage.
Spinal surgery may be a treatment as well. The most important indications for when rheumatoid arthritis is involved are resistant pain, neurologic deficits and/or a need to stabilize the upper cervical spine to prevent spinal cord damage.
References1. Freeman J. RA Facts: What are the Latest Statistics on Rheumatoid Arthritis? Rheumatoid Arthritis Support Network. October 27, 2018. https://www.rheumatoidarthritis.org/ra/facts-and-statistics/. Accessed June 27, 2019.
2. Duarie-Garcia A. Rheumatoid Arthritis. How is rheumatoid arthritis treated? Updated March 2019. https://www.rheumatology.org/I-Am-A/Patient-Caregiver/Diseases-Conditions/Rheumatoid-Arthritis. Accessed June 25, 2019.
Scher JU, Malik F, Manasson J. Using the Microbiome to Aid Psoriatic & Rheumatoid Arthritis Diagnostics & Therapeutics. Rheumatology 2018 Year in Review. https://nyulangone.org/news/using-microbiome-aid-psoriatic-rheumatoid-arthritis-diagnostics-therapeutics. Accessed June 27, 2019.
Talk With Your Doctor
If you have any ongoing symptoms of shoulder pain, its important to share them with your doctor so you can get the right diagnosis. Share with him or her as many details as you can about your symptoms, including when and how long they occur, what the pain feels like , and what you were doing when the pain started.
There are treatment options for both shoulder arthritis and bursitis, so pain relief may be as close as a visit with your doctor.
Recommended Reading: Does Psoriatic Arthritis Itch
Don’t Miss: What Foods Should You Not Eat When You Have Arthritis
Will I Need Surgery For Arthritis
Healthcare providers usually only recommend surgery for certain severe cases of arthritis. These are cases that havent improved with conservative treatments. Surgical options include:
- Fusion: Two or more bones are permanently fused together. Fusion immobilizes a joint and reduces pain caused by movement.
- Joint replacement: A damaged, arthritic joint gets replaced with an artificial joint. Joint replacement preserves joint function and movement. Examples include ankle replacement, hip replacement, knee replacement and shoulder replacement.
Can You Have Fibromyalgia And Ra
Though the conditions are unrelated, having RA may increase a persons likelihood of developing fibromyalgia.
An estimated 2030 percent of people with RA also have fibromyalgia. Researchers suggest that the chronic inflammation and pain associated with RA may make the nervous system hypersensitive over time, leading to fibromyalgia.
Fibromyalgia is more difficult to diagnose than RA because fibromyalgia is diagnosed by exclusion. A doctor will test for many other conditions that cause widespread pain, and if none are present, they may diagnose fibromyalgia.
A doctor will usually diagnose fibromyalgia if:
- a person feels pain when the doctor applies pressure to the 1824 tender points associated with the condition
- symptoms impact all four quadrants of the body
- symptoms have lasted for at least 3 months without a break
Currently, no blood or laboratory tests are used to diagnose fibromyalgia. However, most doctors will order tests, to rule out other conditions, such as arthritis or infection.
If a doctor suspects RA, they will refer the person to a rheumatologist, who specializes in rheumatic conditions. There is no single way to diagnose RA, but the rheumatologist will likely use:
Personal and family medical history. Most people with RA have relatives with the condition, as well as chronic symptoms that impact both sides of the body, primarily the hands and feet.
Imaging tests. X-rays and MRI and ultrasound scans can help to determine if the joints have been damaged.
Don’t Miss: What Foods Cause Arthritis Flare Ups
Chronic Osteoarthritic Pain Causes Brain Changes
Chronic pain in osteoarthritis changes the brain and imparts a unique signature of morphologic or functional characteristics in the brain that may have future clinical implications, according to research presented at the 2011 ACR/ARHP Annual Scientific Meeting held in Chicago in November.
You Might Also Like
A. Vania Apkarian, PhD, a pain researcher and professor of physiology at Northwestern University Feinberg School of Medicine in Chicago, reported his research findings during a presentation entitled Pain, the Brain, and Osteoarthritis. He described an interaction between knee pain and the brain in patients with this chronic disease. The anatomy of the brain in osteoarthritis patients is changing profusely, and it is changing at a rate that we can, in fact, identify, said Dr. Apkarian. The brain as a whole network is reorganizing simply by living with pain.
Using functional magnetic resonance imaging in quantitative psychophysical studies, Dr. Apkarians research team studied brain activity in patients with osteoarthritis. The investigational use of this brain-mapping technique captured brain activity while a mechanical pressure stimulus occurred at the position on the knee where patients complained of pain. Patients also underwent fMRI while they subjectively rated their pain using a visual rating task . The investigators conducted the same experiment in healthy participants.
Studying The Brain In Rheumatoid Arthritis
More specifically, Schrepf and colleagues wanted to see how the peripheral inflammation that is a hallmark of arthritis affects the structure and connectivity of the brain.
To this end, they used functional MRI and structural MRI to scan the brains of 54 participants aged 4366. Brain scans were taken both at the beginning of the study and 6 months later.
The study participants had lived with rheumatoid arthritis for an average period ranging between 2.85 years and over 20 years.
We took the levels of inflammation in their peripheral blood, just as it would be done clinically by a rheumatologist to monitor the severity of their disease and how its being controlled, Schrepf explains.
We found profound and consistent results in a couple areas of the brain that were becoming connected to several brain networks. We then looked again 6 months later and saw similar patterns, and this replication of results is not that common in neuroimaging studies.
To investigate how inflammation affects patterns of functional connectivity in more detail, the researchers examined the connections between 264 brain regions.
You May Like: What Are The Signs Of Rheumatoid Arthritis In Your Hands
Skipping Stretching Is Bad
Regular stretching improves flexibility and eases joint pain. If you do not warm up or stretch before work outs, now is the time to start. It will strengthen muscles and tendons, lubricate joints, and boost your ability to have normal range-of-motion. Ultimately, strong muscles support joint stability, so stretching is a good way to maintain your joint health. Warm up before exercise by doing dynamic or active stretching. This involves doing movements that are similar to those used in the activity or sport that you will be doing. Active stretching boosts blood flow, increases muscle temperature, and gets muscles ready for activity.
Dont Miss: Inflammatory Polyarthritis Symptoms
How Is A Diagnosis Of Rheumatoid Vasculitis Made
The doctor will suspect the diagnosis based on symptoms of rash, numbness or tingling of the hands or feet, skin ulcers, cough and shortness of breath, chest pain, abdominal pain, or stroke symptoms. An electrical test of nerve function is sometimes done to study the numbness and tingling sensations in the arms and legs. Biopsy of the skin or other symptomatic organs is sometimes necessary.
You May Like: What’s The Best Medicine For Rheumatoid Arthritis
Should I See A Doctor
Its common to have aches and pains in your muscles and joints from time to time. This may especially be true if you take part in unusual or strenuous physical activities.
So, how can you tell the difference between the early signs of arthritis and normal pain and stiffness? And, how do you know when you should see a doctor about your symptoms?
If you have swelling or stiffness that you cant explain and that doesn’t go away in a few days, or if it becomes painful to touch your joints, you should see a doctor. The earlier you get a diagnosis and start the right type of treatment, the better the outcome will be.
Here are some other things to think about that might help you decide whether you need to see a doctor: